

Discover more from Social Studies
After nine years as a homeless drug addict in Los Angeles, Jared Klickstein finally checked himself into a drug treatment center. Unlike the program he had gone to six years before, which had hot tubs, acupuncture, and trips to the beach, this one, in North Hollywood, was deadly serious about personal responsibility. Clients kept a strict schedule. They did chores. They scrubbed toilets. “No hot tubs,” Klickstein said.
Most importantly, they couldn’t use drugs. “If you use, they kick you out,” he said. “There’s consequences.”
It took him two attempts, but Klickstein, now 33, finally got clean. Four-and-a-half years later, he’s independent, employed and emotionally stable. “I was a person that you would see on one of these videos, screaming with blood and shit all over them,” he said. “And now I’m not.”
Klickstein attributes his success to the North Hollywood program’s emphasis on sobriety and accountability. “Without sobriety, there is no mental or emotional stability for me and most other drug addicts, meaning homelessness was inevitable,” he said. “Half measures and coddling do not work. Period.”
But tough-love centers like the one that turned Klickstein’s life around are becoming harder to come by. The idea that you have to quit drugs to recover from addiction has become old-fashioned, and treatment centers that insist on abstinence are disappearing. In California, changes in state law have made it virtually impossible for any program that accepts public funds to push clients to quit using.
“You cannot intervene or even speak to someone regarding their alcohol and drug use,” said Reverend Andy Bales, who has worked in drug recovery in Los Angeles for decades. As a result, most homeless services and housing providers in the city allow, in his words, “a free flow of alcohol and hard drugs.” This permissive approach, Bales believes, is why California has more people living on the street than any other state in the country.
The repudiation of abstinence-based treatment in California and many other states represents the broad embrace of an approach called “Harm Reduction.” Instead of seeing addiction as a serious illness whose treatment ultimately requires addicts to stop using drugs, it casts addiction as a risky health condition to be managed, and insists that different people benefit from different management strategies, not all of which require abstinence.
In 2016, proponents of Harm Reduction succeeded in getting their approach codified into California law. To be eligible for state funding, facilities that house or treat homeless addicts are prohibited from making their services contingent upon sobriety. That has put service providers that depend on public funding — those that don’t cater to clients with private insurance and that aren’t philanthropically funded — in a difficult position. Increasingly, programs that once required sobriety have switched up their treatment modalities and are now more permissive toward continued substance use. Out of several dozen treatment and housing programs on L.A.’s Skid Row, Bales estimates that you could count the number that are still abstinence-based on one hand.
Bales’ center, the Union Rescue Mission, has foregone public funding in order to remain abstinence-based. “It’s gotten really tough to be a person focused on recovery, when it seems every agency around me on Skid Row has given into the Harm Reduction model,” he said.
No single drug treatment method works for everyone, and that includes abstinence. While some, like Klickstein, need total sobriety, others may be capable of becoming functional and healthy while still using — for instance, by switching from methamphetamines to cannabis, or from heroin to methadone. Whatever treatment approach works for a given addict, harm reduction, as it is traditionally understood, buys them the time to find it and succeed in it, simply by keeping them alive.
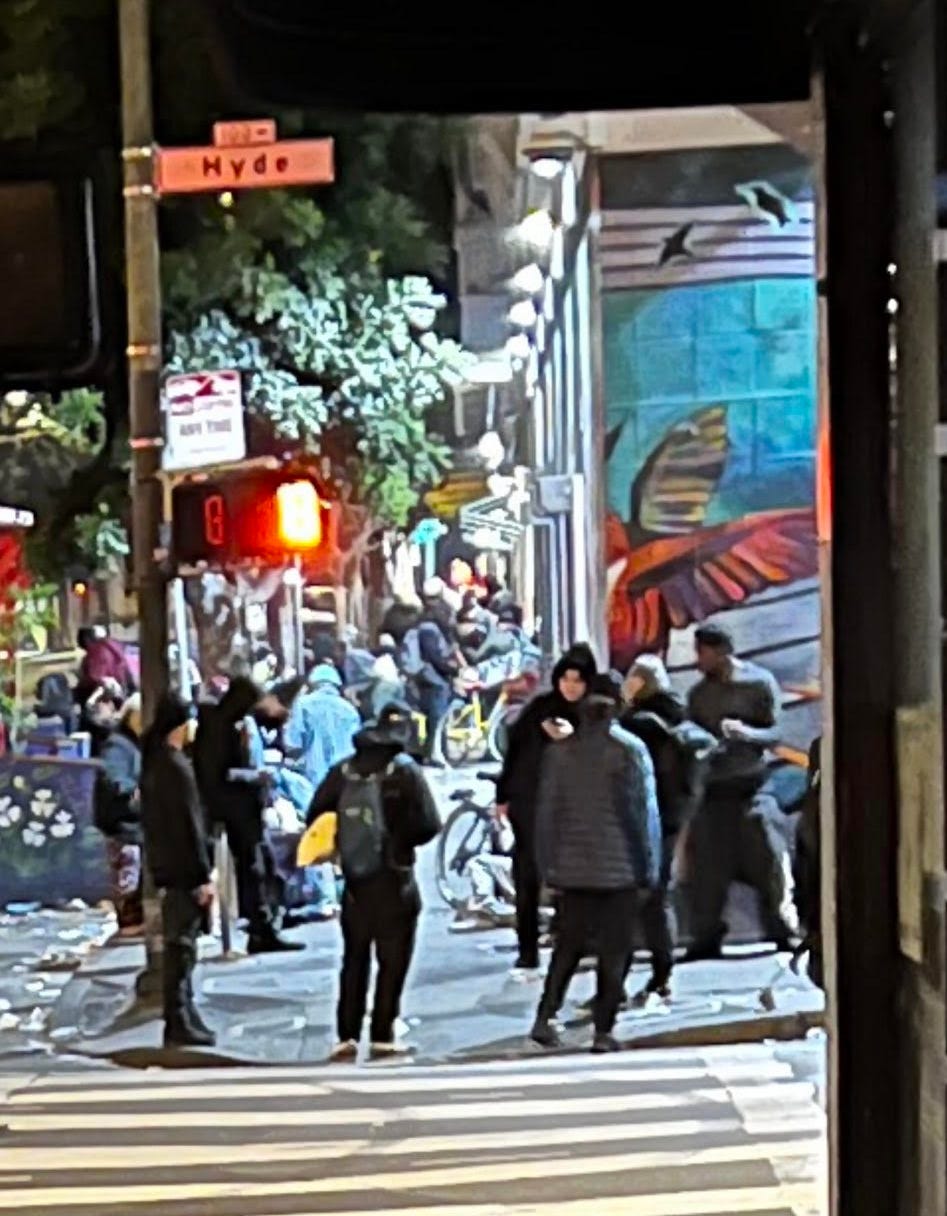
But as the addiction crisis has deepened across the country, with the highly toxic and addictive opioid fentanyl killing addicts at record rates, homelessness exploding in California and throughout the West Coast, and drug cartels operating in the open in cities like San Francisco, the ascendance of a particularly dogmatic form of harm reduction may be exacerbating the crisis instead of mitigating it. By normalizing drug use, eschewing intervention and shutting down abstinence-based treatment programs, critics of this radical harm reduction philosophy believe it’s keeping people trapped in addiction.
“It’s just going to end up with more death,” said Klickstein.
Harm Reduction
The Harm Reduction model emerged roughly four decades ago when it served as the philosophical underpinning of needle exchange programs. The idea then was that since most people who are addicted to heroin are going to continue using it for some period of time, they should be kept safe. “You can’t get people to recover if they’re dead,” Dr. John Rotrosen, a psychiatrist specializing in addiction research at New York University, told RCI. By distributing clean syringes, not only were users protected from blood-borne illnesses, but the public was also protected from outbreaks of diseases like Hepatitis-C and HIV.
The approach has evolved. Over time it expanded to include relatively non-controversial tools that better fit the mix of drugs on the streets today, such as the mass distribution of Naloxone, a medication for opioid overdoses, and of test strips that measure the presence and amount of fentanyl in drug samples. But it has also adopted certain social philosophies around drug use that go well beyond these pragmatic, life-saving tools.
“Some people have taken it to the extreme,” Dr. John Kelly, a Harvard psychiatrist who specializes in addiction, told RCI. “Ideas of social justice have been infused into this debate, which are separate from the clinical issues.”
Today, the most radical advocates of harm reduction don’t see drug use, in and of itself, as a problem. Rather, they view the risks that accompany it – which, from their perspective, can be effectively mitigated – and drug enforcement as the harms to be reduced. Some denounce programs like Bales’ both because they require participants to be clean and because they define long-term sobriety as the necessary end goal of treatment. Some support full drug legalization and government-provided drugs on demand. In Vancouver, the city is already administering fentanyl to addicts, paid for by the Canadian government. The goal, from this perspective, is not necessarily sobriety. It’s simply longevity.
Sally Satel, an addiction psychiatrist, calls this version of the philosophy “subsistence harm reduction” — as in, the goal is simply to survive in one’s addiction — as opposed to the traditional, 1980s-era ”aspirational harm reduction” — as in, one aspires to get sober.
“It’s become this buzz phrase,” said Troy Vaughn, a pastor and a former homeless drug addict who runs the Los Angeles Mission. “People think harm reduction is you can let somebody come into your place and do whatever they want to without consequences. Harm reduction doesn’t mean no rules.”
Safe Consumption
In San Francisco, as in Los Angeles, “subsistence harm reduction” has become the principal public health approach to the addiction crisis. In January, the Mayor and the Department of Public Health opened the “Tenderloin Linkage Center,” a site where addicts could use drugs under the supervision of city officials and city contractors armed with Naloxone in case of overdoses. Harm reduction advocates believe that “safe consumption sites” like the Tenderloin Linkage Center are indispensable to saving drug users’ lives from fatal overdoses, and have sought to open more of them throughout California.
The city promoted the center as a place where users could be connected to services, including drug treatment for those who wanted it. Out of approximately 110,600 visits, however, only 1,861 people requested treatment services – fewer than 2% of the center’s visitors.
“You can buy drugs across the street and use them inside. Why would anyone want to get clean under those circumstances? What's the incentive?” asked Tom Wolf, a recovering addict who once lived on the streets and now advocates for abstinence-based recovery. He believes the Tenderloin Linkage Center, which Mayor London Breed is shutting down next month in the face of widespread criticism of the flocks of drug dealers it has attracted, made the addiction crisis worse.
Supporters of facilities like the Tenderloin Linkage Center argue that, in addition to keeping users alive in the short term by having people on hand to save them from overdoses, there’s value in building rapport between service providers and drug users that can be leveraged down the road to coax people into treatment. In many cases, treatment isn’t needed at all to achieve an end to drug use. “Most people who end up with substance use disorders quit without any treatment – through family pressure, or through other relationships,” said Beau Kilmer, a drug policy researcher at the RAND Corporation. For those users, simply keeping them alive long enough to decide to quit on their own is enough.
A 2012 study that Maia Szalavitz, perhaps the most prominent harm reduction advocate in the United States, has trumpeted, bears out Kilmer’s observation. That study, however, did not look at users of fentanyl, which kills much faster than other narcotics. While most cocaine addicts, according to the study, quit on their own within five years of becoming addicted, fentanyl addicts or users of drugs laced with fentanyl may not have that long to wait. Without intervention, they’re more likely than users of other drugs to die before they summon up the resolve to kick the habit. And since fentanyl is in basically every street drug today, there effectively are no “other drugs” anymore. Every addict is in this risk category.
“I’m insanely lucky I stopped right when fentanyl came in full force,” said Klickstein. “The way I get high, I’d absolutely be dead.”
Intervention
If Klickstein had been allowed to continue to use and to commit the crimes that supported his habit with impunity, he believes he would not have survived. Instead, he was arrested, after another homeless man attacked him at a Panda Express, and he pulled a knife in retaliation. He ended up spending six months in jail, where he kicked his heroin habit. Though he relapsed a couple of times after getting out, he never became addicted again. “It was all I could ask for,” he said. “It was the greatest thing that ever happened to me.”
It’s a common refrain from recovered addicts: many believe they never could have gotten clean without the forced respite from drug use of a jail sentence.
Achieving that benefit doesn’t necessarily require jail, however. The purpose of drug courts is to impose drug treatment by force on those unwilling or incapable of seeking it, but without having to resort to the brute force of the criminal justice system.
That too, however, is met with staunch opposition from harm reduction advocates, who often claim that involuntary treatment simply “doesn’t work.” Szalavitz, for instance, wrote a New York Times op-ed earlier this year entitled “Why Forced Addiction Treatment Fails.”
The research, however, paints a muddier picture. Dr. John Kelly, the Harvard psychiatrist, has investigated the question of involuntary versus voluntary treatment. “When people are involuntarily committed, they don’t do worse,” he said. “They do as well.”
In an age of fentanyl, there may not be time to wait for addicts to decide to quit, and the longer their addictions persist, the bigger a toll it takes on their long-term health. “If we mandate treatment, it’s not perfect,” said Sheldon Bailey, a former addict and recovery advocate in Alberta, Canada. “But it’s better than ending up dead.”
Stigma
Another part of Klickstein’s success that harm reduction proponents wish to eradicate is the social stigmatization of drug use.
One of the core tenets of harm reduction philosophy is that stigma makes addiction worse by discouraging users from seeking help. It’s a supposition that has been borne out by scholarly research. Accordingly, the thinking goes, we should seek to de-stigmatize drug use as much as possible. The unofficial slogan of the harm reduction movement is to “meet people where they’re at” – meaning that you work with people in whatever condition they’re in, rather than putting expectations on them of how you think they should be. Supervised consumption sites, for instance, are designed, in part, to create a place where people can use drugs without feeling judged or pressured to change.
But by not placing different expectations on drug users – expectations of sobriety, of personal responsibility, of productivity – proponents of recovery argue that society is in effect telling addicts that this is all they’ll ever be, and that they shouldn’t expect or feel obligated to change.
“People say stigma is bad. Stigma is not bad,” said Keith Humphreys, a psychologist who specializes in addiction and served as a senior advisor in the Obama administration. “When I was young, people joked about drunk driving and domestic violence. It wasn’t stigmatized – it was like, ‘That’s Otis for ya!’ These things have become deeply stigmatized over my lifetime.”
To break people out of their dependencies, Satel insisted, you don’t normalize their behaviors – you change them. “You start out with rules: Don’t drive past the dealer's house. Have your paycheck direct deposited. Change friends,” she said. “A lot of it is just binding yourself to the mast.”
This was what Klickstein’s treatment center did for him. “Strict rules, pride in following the rules and disdain for those that broke them” all helped show him he could determine the course of his own life. Even more important than that was the change in the people around him. “I was suddenly surrounded by a hundred people who were clean,” he told me, “and was essentially forced into having dozens of friends that were clean.”
Sites like the Tenderloin Linkage Center do the opposite. “Supervised consumption sites connect you with other people actively using,” he said.
Medication
Harm reduction advocates are generally enthusiastic proponents of methadone and buprenorphine, which are clinically-administered opioids that forestall withdrawal symptoms from heroin and fentanyl, making it easier for addicts to be successful in their drug treatment programs.
There’s a broad consensus among addiction treatment experts in favor of the use of methadone and buprenorphine (brand name Suboxone), whether they believe in abstinence-based recovery or in harm reduction. It’s an indispensable tool to stabilize people enough to focus on things other than their next fix and start to make better choices. As a bridge to sobriety, it’s an integral part of many abstinence-based programs.
“It was the first time in my life where I wasn’t thinking about using, and it gave me the time to get other shit in my life in order – like with my family, get stable, gain weight, starting to build my body back up,” said Lauren Schiro, who spent years living on the street in Los Angeles before going on methadone and is now in recovery.
There are, however, knock-on effects to this treatment that compound the harms of the drug trade.
One problem is that many active users take methadone not in substitution but in addition to their drug of choice, in order to prevent withdrawal when they can’t find heroin or fentanyl, according to Schiro. For that reason, there’s a black market for methadone, and users are able to sell it for drugs.
Another problem is that, as an opioid, methadone is addictive, so once you’re on it, you may be on it for the rest of your life.
Klickstein believes harm reduction proponents are being cavalier with their unquestioning embrace of methadone and Suboxone. “It’s like, well let’s just get everyone on Suboxone or methadone or whatever. Let them quit at their own rate,” he said of the harm reduction approach. “We're talking about kids that are 20 to 25 years old. Like you're just going to throw in the towel and get on methadone for the rest of your life?”
“Using an addicting drug to treat addiction is very problematic,” said Dr. Percy Menzies, who founded and runs a drug treatment center in Saint Louis. “No chronic condition can be successfully treated with an addicting drug.”
In his program, Menzies prescribes Naltrexone, a drug with the opposite effect of methadone and buprenorphine: it prevents you from being able to get high. After a user detoxifies with the assistance of methadone or buprenorphine, they can get a shot of Naltrexone that lasts 28 days. During that time, they have no option to get high, and therefore cannot relapse.
Very few recovered addicts I’ve spoken to have ever been prescribed Naltrexone, and despite its efficacy, it is rarely mentioned in the public discourse around the addiction crisis. Menzies believes this is due to the lobbying power of the methadone clinics, which have refused to adopt it. “The methadone clinics needlessly saw Naltrexone as an existential threat,” said Menzies.
Since Naltrexone is a tool to achieve sobriety, it has come to be erroneously perceived as a medication for only highly motivated addicts, according to Menzies. “For healthcare professionals, it is for business executives, it is for well-to-do people,” he said of this popular misconception. “Naltrexone for the well-to-do people; the rest get methadone.”
This two-tier treatment regime is one example of how, in Menzies’ opinion, the current system is betraying low-income drug users by expecting less of them than they’re actually capable of. By telling addicts they have a chronic condition to be managed over a lifetime instead of showing them there’s a way out of their addiction, low expectations serve the business model of the treatment industry.
“The addiction medicine industry is still heavily based on the commercial model of treatment,” he said. “They continue to describe addiction as an incurable disease. And that gives people no hope.”
Recovery
Reverend Bales likewise believes that drug addicts are being betrayed by the rigid harm reduction treatment model. “I’d say L.A., and the West Coast of the United States, and British Columbia, Vancouver – they believe in ‘meeting people where they are’ and leaving them there to die,” he said.
But as Vaughn pointed out, abstinence and harm reduction were never mutually exclusive. They’re polarized in practice, but there’s nothing inherently incompatible about them. In California, addiction treatment service providers who believe in both models are trying to figure out how to strike a balance, even with laws on the books that restrict their options. “How can we honor the framework of harm reduction, but also offer everything within our power to help people break free from addiction?” asked Ken Craft, Founder and CEO of Hope of the Valley, a treatment center in Los Angeles, which, as a recipient of public funds, employs the harm reduction standards required by the state.
“We need to be able to allow organizations to interpret harm reduction,” said Vaughn. “We can’t say abstinence is not a part of harm reduction.”
Subscribe to Social Studies
Politics, media and social theory

















One of the great ironies here is that the Social Justice religion, which places the Victim (of anything and everything from "historical forces" to "power differentials" to that evil mark of Cain they call "Stigma") at the center of its movement and which is to California what Catholicism is to Rome, will end up killing many more of its sacred Victims than would have died or suffered otherwise.
I've said here before that I lived four years recently in Venice, CA, and I've seen all this up close: Social Justice disciples will vehemently furiously denounce anyone or anything in the most unhinged language if they suggest even one limit to the rights of junkies to do as they please at all times (thus meaning junkies' rights become paramount in any situation), even if this supposed right has the same result as giving a bottle of whiskey to a drunk or a bucket of KFC to someone morbidly obese.
The Social Justice religion has conquered the world because it allows people and organizations and esp politicians to purchase virtue on the cheap, with other people paying the price. But often the most compassionate thing you can do for people is to say NO. Otherwise your "compassion" is really about making yourself feel (and be seen as) good, world be damned.
As much as any opiate or fentanyl, the Social Justice religion's potent hit of self-righteousness, of making its users feel higher than anyone else when it comes to Caring and Being on the Right Side of History™, is the true Californian epidemic and I don't know if there will be any cure in our lifetimes.
Harm reduction and low/no barrier housing are why Seattle and San Francisco and other like minded cities are the hell holes they are today. Some things are just not okay, like defecating in public or pitching your tent next to an elementary school while you pursue your drug-addicted "freedom" to live however you want. I wouldn't wish the life of an addict in one of these 'caring' cities on my worst enemy. If we really cared, we'd say no. No we won't affirm your throwing away the one precious life you have. No we won't watch you rot out your body and soul while you slowly die right in front of us. Harm reduction doesn't save lives, all it does is extend a miserable existence for a few more days or months or years. By the way, Vancouver BC, a pioneer in harm reduction, had the most ever overdose deaths in the first 9 months of 2022.